Abstract
Introduction
Asplenia, the absence of normal spleen function, may be congenital or acquired (Rubin & Schaffner 2014). The spleen plays an important role in immune response, particularly in the filtration of encapsulated bacteria (Brown et al. 1981). Asplenia renders patients with this condition at risk of life threatening bacterial infections (Winkelstein 1977). Overwhelming post-splenectomy infection (OPSI) has a mortality rate of 50% (Bisharat et al. 2001). In an observational study conducted over 4 years, 72 cases of potentially preventable OPSI were reported in patients aged 3 months to 87 years (Waghorn 2001). In this study, 74% of patients were not prescribed antibiotics (neither prophylactic nor for treatment use), 69% had not received the pneumococcal vaccination and only 1 of 77 individuals was issued a medical alert card for asplenia.
The objective of our study was to enhance recognition and understanding of asplenia as well as to promote appropriate preventative measures for infection for people with asplenia at St. Michael's Hospital in Toronto, Canada.
Methods
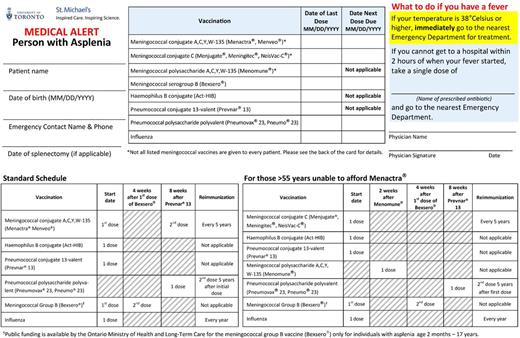
A prospective quality improvement study was conducted over one year in the hematology clinics at St. Michael's Hospital. An interdisciplinary team of stakeholders were engaged and provided strategies to enhance the medical management of patients with asplenia. A medical alert card and educational booklet for patients with asplenia were developed. The medical alert card was used to record vaccination status and educate the patient to present immediately to medical attention at the onset of fever. The booklet described the importance of immunization and the symptoms indicating the onset of a potentially life-threatening infection. It also outlined vaccination schedules and management of fever for patients with asplenia. The booklet was directed towards both patients and clinicians.
We administered a baseline questionnaire to patients with asplenia who presented to the hematology clinic. The questionnaire measured patients' understanding of asplenia. Following the questionnaire, the medical alert the card and booklet were distributed to the patients with asplenia. A follow-up questionnaire was completed by the patient at their next presentation. The primary outcomes included change in number of patients aware of their: condition, vaccination record; appropriate fever management; and prescribed antibiotic. Secondary outcomes included: change in vaccination rates and patient satisfaction.
This initiative was formally reviewed and approved by Quality Improvement authorities at St. Michael's Hospital.
Results
Thirty patients with asplenia completed the baseline questionnaire. Sixty-seven percent of patients had an unknown or incomplete vaccination record, 82% were unaware that fever requires immediate medical attention and 100% were unaware of a prescribed antibiotic in the event of fever if more than 2 hours away from medical attention. Of the 30 patients with asplenia who received the medical alert card and booklet, 20 (67%) have completed the follow-up questionnaire. 17/20 (85%) were informed regarding their vaccination status and 15/20 (75%) were either completely vaccinated or were taking measures to become appropriately vaccinated. 15/20 (75%) demonstrated an improved understanding of appropriate fever management.
Conclusions
The implementation of a personalized medical alert card and booklet is associated with improved awareness and understanding of asplenia and its consequences. We anticipate these preventative measures will empower patients to facilitate their safe medical care. Given the successful outcomes and apparent need, we are extending this intervention to other areas of St. Michael's Hospital and beyond.
Sholzberg: Shire: Honoraria, Research Funding; CSL Behring: Honoraria, Research Funding; Octapharma: Honoraria, Research Funding; NovoNordisk: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal